Surprising results from a recent study show that TV food commercials set off a region of the brain that controls the mouths of overweight teens, stimulating unhealthy eating habits.
A Dartmouth study finds that TV food commercials disproportionately stimulate the brains of overweight teen-agers, including the regions that control pleasure, taste and — most surprisingly — the mouth, suggesting they mentally simulate unhealthy eating habits.
The findings suggest such habits may make it difficult to lose weight later in life, and that dieting efforts should not only target the initial desire to eat tempting food, but the subsequent thinking about actually tasting and eating it – in other words, you should picture yourself munching a salad rather than a cheeseburger.
The study appears in the journal Cerebral Cortex. A PDF is available on request. The study included researchers from Dartmouth College’s Department of Psychological and Brain Sciences and the Norris Cotton Cancer Center at the Dartmouth-Hitchcock Medical Center and Geisel School of Medicine at Dartmouth.
The prevalence of food advertising and adolescent obesity has increased dramatically over the past 30 years, and research has linked the number of television shows viewed during childhood with greater risk for obesity. In particular, considerable evidence suggests that exposure to food marketing promotes eating habits that contribute to obesity.
Continue Reading Below ↓↓↓
Using functional magnetic resonance imaging, the Dartmouth researchers examined brain responses to two dozen fast food commercials and non-food commercials in overweight and healthy-weight adolescents ages 12-16. The commercials were embedded within an age-appropriate show, “The Big Bang Theory,” so the participants were unaware of the study’s purpose.
The results show that in all the adolescents, the brain regions involved in attention and focus (occipital lobe, precuneus, superior temporal gyri and right insula) and in processing rewards (nucleus accumbens and orbitofrontal cortex) were more strongly active while viewing food commercials than non-food commercials.
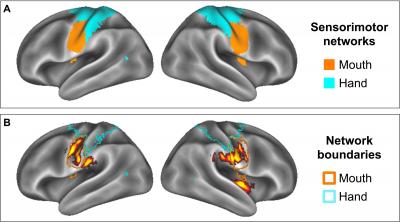
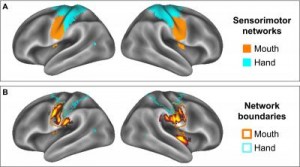
Also, adolescents with higher body fat showed greater reward-related activity than healthy weight teens in the orbitofrontal cortex and in regions associated with taste perception. The most surprising finding was that the food commercials also activated the overweight adolescents’ brain region that controls their mouths. This region is part of the larger sensory system that is important for observational learning.
“This finding suggests the intriguing possibility that overweight adolescents mentally simulate eating while watching food commercials,” says lead author Kristina Rapuano, a graduate student in Dartmouth’s Brain Imaging Lab. “These brain responses may demonstrate one factor whereby unhealthy eating behaviors become reinforced and turned into habits that potentially hamper a person’s ability lose weight later in life.”
Although previous studies have shown heightened brain reward responses to viewing appetizing food in general, the Dartmouth study is one of the first to extend this relationship to real world food cues — for example, TV commercials for McDonald’s and Burger King — that adolescents encounter regularly. The brain’s reward circuitry involves the release of dopamine and other neurotransmitter chemicals that give pleasure and may lead to addictive behavior.
Children and adolescents see an average of 13 food commercials per day, so it isn’t surprising they show a strong reward response to food commercials. But the new findings that these heightened reward responses are coupled with bodily movements that indicate simulated eating offer a clue into a potential mechanism on how unhealthy eating habits are developed.
“Unhealthy eating is thought to involve both an initial desire to eat a tempting food, such as a piece of cake, and a motor plan to enact the behavior, or eating it,” Rapuano says. “Diet intervention strategies largely focus on minimizing or inhibiting the desire to eat the tempting food, with the logic being that if one does not desire, then one won’t enact. Our findings suggest a second point of intervention may be the somatomotor simulation of eating behavior that follows from the desire to eat. Interventions that target this system, either to minimize the simulation of unhealthy eating or to promote the simulation of healthy eating, may ultimately prove to be more useful than trying to suppress the desire to eat.”
Source: Dartmouth College
Journal: Cerebral Cortex