Another diabetes drug is coming under fire, this time for the dramatic influence it has on bone health by substantially increasing bone fat and thus the risk of bone fractures. Even worse, a new crop of similar drugs will have the same problem.
Inside our bones there is fat and diabetes increases the amount of this marrow fat. A study from the UNC School of Medicine now shows how some diabetes drugs substantially increase bone fat and thus the risk of bone fractures.
The study, published in the journal Endocrinology, also shows that exercise can decrease the volume of bone fat caused by high doses of the diabetes drug rosiglitazone, which is sold under the brand name Avandia.
“These drugs aren’t first or second-line choices of treatment for type-2 diabetes, but some patients do take them,” said study first author Maya Styner, MD, assistant professor of medicine. “And we know there are drugs in development that target the same cellular pathways as rosiglitazone does. We think doctors and patients need to better understand the relationship between diabetes, certain drugs, and the often dramatic effect on bone health.”
According to Styner’s study, rosiglitazone affects bone fat by enhancing a critical transcription factor called PPAR – peroxisome proliferator-activated receptor – which regulates the expression of specific genes in the nuclei of cells. Essentially, rosiglitazone takes glucose out of blood to lower blood sugar and treat diabetes. But that glucose is then packaged into lipid droplets – fat. Other researchers showed that some of that fat is stored in tissue, such as belly fat. Styner’s latest research showed that the drug also causes fat to be stored inside bone.
Continue Reading Below ↓↓↓
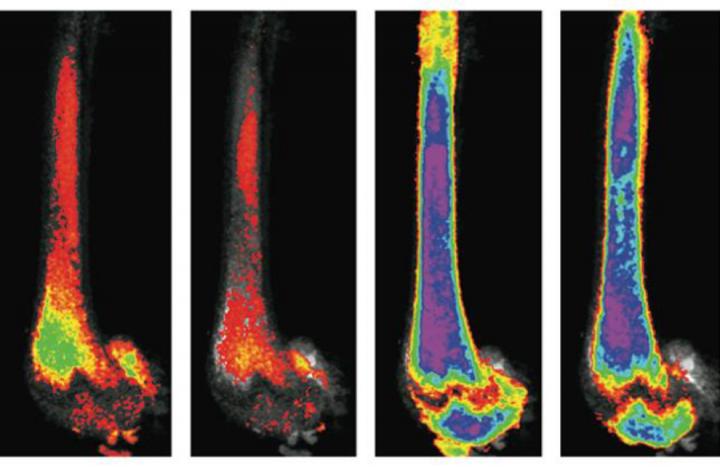
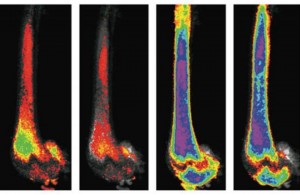
“First, we were surprised by the massive amount of bone fat caused by rosiglitazone,” Styner said. “The images were just stunning. Also, the drug is so powerful and we used such a high dose that we didn’t think exercise would decrease the fat depot much, if at all. But exercise did decrease the volume of bone fat by about 10 percent, which was similar to the decrease we reported seeing in mice that were not given the drug but were instead fed a high-fat diet.”
Styner said that many of her patients have been surprised to learn that some diabetes drugs can adversely affect bone health. She also said that diabetes itself can harm bones.
Avandia fell out of favor about a decade ago because of heart-related side effects. Physicians can still prescribe the drug, but it isn’t as popular as it once was. Its cousin pioglitazone is also still available and has been shown to cause fewer heart-related side effects, Styner said, but it also isn’t used as a first or second-line drug to treat diabetes.
Yet, other drugs under development that could be close to FDA-approval lower blood sugar by enhancing the PPAR pathway. These drugs are referred to as fibroblast growth factor-21 agonists.
“Early reports show that the same bone concerns are popping up with these new drugs,” Styner said. “Doctors and patients need to be aware of this.”
Bone fat, in general, isn’t nearly as well understood as other fat depots.
“Our field is just beginning to investigate bone fat and its implications for patients,” Styner said. But she said that more bone fat means less actual bone, which increases the risk of bone fractures.
All of us have fat in our bones. It’s just a matter of how much. Styner said that the same kind of stem cell in our marrow creates bone cells and fat cells. Previously, Styner used a new osmium staining technique to visualize that a high-fat diet increases the fat depots in the bones of mice, just as a high-fat diet increases belly fat.
There are still differing theories for how bone fat increases due to a high-fat diet and how exercise lowers it. Styner said exercise might trigger marrow stem cells to create more bone cells instead of fat cells. Or perhaps exercise causes the body to access bone fat as fuel.
“It could be that bone fat is just another depot, a good energy store that allows bone cells to do what they need to do so bones become stronger,” Styner said.
Continue Reading Below ↓↓↓
Whatever the case, exercise aids bone health. In her studies, Styner’s team added a running wheel to mouse cages. Mice are natural runners. At night, they’d run several miles on the wheel. Styner’s team then measured the effects of running. (see images) Even on a high dose of a power drug, such as rosiglitazone, the mice that exercised showed a significant decrease in bone fat.
Styner said her findings are not yet directly relatable to human activity. For humans, running isn’t nearly as natural. But she said she would still advise patients at risk of declining bone health to find an exercise that suits them; the default would be taking very long walks.
Also, Styner is hoping to work with exercise scientists at UNC-Chapel Hill to use advanced MRI technologies to visualize the effects of exercise on human bone health.
The National Institutes of Health funded this research. Janet Rubin, MD, professor of medicine and pharmacology, is the senior author of the paper that appeared in the journal Endocrinology.
Source: University of North Carolina Health Care
Journal: Endocrinology
Funder: National Institutes of Health
Photo Credit: UNC School of Medicine