March 2011 - Transplanting human umbilical cord blood-derived endothelial progenitor cells (EPCs) has been found to "significantly accelerate" wound closure in diabetic mouse models, said a team of Korean researchers publishing in the current issue of Cell Transplantation (19:12), now freely available online.
According to the study's corresponding author, Dr. Wonhee Suh of the CHA University Stem Cell Institute, diabetes is often associated with impaired wound healing. While the therapeutic potential of transplanted EPCs has been demonstrated in animal models and in humans who have suffered stroke, myocardial infarction and peripheral artery disease, their effect in healing stubborn wounds has not been studied to the same degree.
"EPCs are involved in revascularization of injured tissue and tissue repair," said Dr. Suh. "Wounds associated with diabetes that resist healing are also associated with decreased peripheral blood flow and often resist current therapies. Normal wounds, without underlying pathological defects heal readily, but the healing deficiency of diabetic wounds can be attributed to a number of factors, including decreased production of growth factors and reduced revascularization.
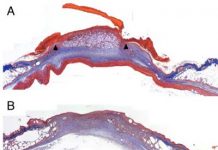
The researchers, who transplanted EPCs into an experimental group of mice modeled with diabetes-associated wounds, but did not transplant EPCs into a control group, found that the EPCs "prompted wound healing and increased neovascularization" in the experimental group.
"The transplantation of EPCs derived from human umbilical blood cells accelerated wound closure in diabetic mice from the earliest point," said Dr. Suh. "Enhanced re-epithelialization made a great contribution in accelerating wound closure rate."
Continue Reading Below ↓↓↓
The researchers found that growth factors and cytokines (small proteins secreted by specific cells of the immune system) were "massively produced" at the wounded skin sites and contributed to the healing process.
"It remains unclear, however, which mechanism plays the dominant role in EPC-mediated tissue regeneration," commented Dr. Suh. "Further study is required since numerous studies have shown that the actual magnitude of EPC incorporation into the vasculature varies substantially from study to study."
"This experimental study opens the possibility of the future clinical use of endothelial progenitor cells derived from human cord blood in the treatment of diabetic wounds in humans" said Prof. Voltarelli, Professor of Clinical Medicine & Clinical Immunology at the University of Sao P�ulo, Brazil and section editor for Cell Transplantation . "Interestingly, it also shows that the culture medium used to grow the cells (conditioned media) has the same healing effect as the cells, so that it could be used as a cell-free form of treatment."
Citation: Kim, J. Y.; Song, S-H.; Kim, K. L.; Maeng, Y-S.; Im, J-E.; Yie, S. W.; Ahn, Y. K.; Kim, D-K.; Suh, W. Human Cord Blood-derived Endothelial Progenitor Cells and their Conditioned Media Exhibit Therapeutic Equivalence for Diabetic Wound Healing. Cell Transplant. 19(12):1635-1644; 2010.
Source: Cell Transplantation Center of Excellence for Aging and Brain Repair