February 2003 � A new optics technology is providing scientists with real-time microscopic images of the living retina, and may allow doctors to focus in on earlier diagnosis and treatment of diseases such as diabetes and glaucoma.
University of Houston researchers are using a technology called adaptive optics to peer inside the eyes of human subjects and for the first time get clear, sharp images of features such as blood flow in the eye�s retina. Until now, clear images of the living retina were not possible because the eye�s own structure interferes with the imaging process.
"Everyone suffers from natural irregularities in the cornea and lens of the eye, and even in people with normal, 20/20 vision, these defects prevent the eye from focusing light from the world into a nice sharp image on the retina," says Austin Roorda, assistant professor of optometry at the University of Houston. "Eye doctors have to look through these same defects when they examine a patient�s retina, and the image they see is not very clear, limiting the amount of information they can get."
A clear view of the retina is key to the early diagnosis of diseases such as glaucoma, which produces changes in the nerves in the eye, and diabetes, which affects blood flow in the retina.
"The eye is a wonderful instrument, but its optics are not particularly good, and this has limited our ability to clearly see what�s happening in there," Roorda says.
Continue Reading Below ↓↓↓
Using adaptive optics, researchers accurately measure the defects in the cornea and the lens and compensate for them to produce detailed microscopic images and video of human retinas. In his lab, Roorda and his colleagues have built a scanning laser ophthalmoscope, the only device of its kind that incorporates adaptive optics.
"We get a much clearer picture of the retina than any other technology can produce, with the added advantage that the data we get is in real time," Roorda says.
Roorda�s scanning laser ophthalmoscope won�t be in clinics any time soon, but he says it�s a prototype for the next generation of such devices. He and colleagues at four other institutions, led by the University of Rochester, recently received a $10 million, five-year grant from the National Institutes of Health to build more adaptive optics devices.
Roorda will present information about his research Feb. 16 in Denver at the annual meeting of the American Association for the Advancement of Science.
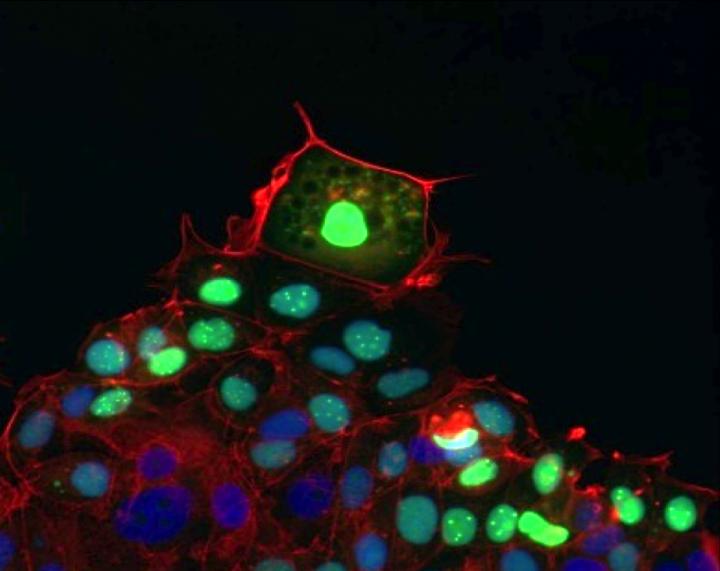
During the past year, Roorda has examined normal eyes in about 30 people, and four people with medical conditions that affect the eyes. He and his UH team have seen capillaries � the smallest blood vessels in the retina � and the white blood cells flowing through them. Tracking the movement of white blood cells helps them measure the rate of blood flow, as well as monitor their specific behavior.
"Right now we�re focusing on understanding what normal eyes look like with this instrument. This is a whole new view of the retina, and we�re developing protocols for imaging patients," Roorda says.
The UH researchers are working with a physician at the Texas Medical Center and plan to look at patients with diabetes, for example, to examine their blood flow dynamics. In diabetics, it is thought that white blood cells tend to be sticky and may move differently through the capillaries than they do in normal retinas. Roorda�s team also plans to look at glaucoma patients, whose retinal nerves have been changed by the disease, and people with changes or losses in their cone photoreceptors.
"We should be able to watch the progression of these types of diseases," he says.
In the lab, Roorda�s test subject sits in front of the device, and his head is kept still by having the person bite down on a custom-fit mouthpiece mounted in place. The adaptive optics setup involves shining a weak laser into the subject�s dilated eye. The laser light reflects off the retina and is scattered back out of the eye, where it is picked up by a wavefront sensor. This component measures the defects in the lens and cornea and feeds that information back to a deformable mirror, which is the backbone of the device.
"The mirror is made of glass, which is flexible, and it is supported on its back surface by a grid of electronically controlled small pistons that ever-so-slightly change the mirror�s shape in such a way as to focus the scattered light into parallel rays. This, and a lot of sophisticated computer code, is what then produces the clear, corrected image," Roorda says.
Continue Reading Below ↓↓↓
One of the future clinical applications of Roorda�s device might be microretinal surgery, where surgeons need a clear view of an area they would like to treat.
"The way we use our laser to scan the retina to produce an image, it may be possible to use the technique for treatment. While you�re imaging a microaneurysm, for example, if we could track that feature we may be able to then turn on a treatment laser and blast it with the same precision that we can see it," he says.
Roorda earned his Ph.D. in physics at the University of Waterloo in Canada and began his work in adaptive optics as a post-doctoral researcher at the University of Rochester. He joined the UH faculty in 1998. His research is funded by the National Institutes of Health, as well as by the National Science Foundation through the Center for Adaptive Optics at the University of California at Santa Cruz.
Source: University of Houston