July 2005 - In the July issue of Cell Metabolism, researchers report the discovery of a trigger for insulin resistance in the liver. Hepatic insulin resistance is a silent condition that increases the chances of developing diabetes and heart disease. The team's findings also identify a potential target for drugs to prevent or treat the condition, the researchers said.
The livers of mice lacking an enzyme called mitochondrial acyl-CoA:glycerol-sn-3-phosphate acyltransferase 1 (mtGPAT1) remain sensitive to insulin's effects when fed a high-fat diet. The mice also exhibit lower concentrations of a lipid metabolite that might play a key role in triggering the liver to become insulin resistant, the researchers found.
Along with the existing epidemic of obesity, fatty liver, also known as hepatic steatosis, is rapidly becoming a major health care problem, said Howard Hughes Medical Institute investigator Gerald Shulman of Yale University, senior author of the study. Fatty liver can lead to altered liver function, elevated lipids such as cholesterol and triglycerides in the bloodstream, and progression to liver cirrhosis, he said. Characterized by scarring, cirrhosis of the liver is the twelfth leading cause of death by disease, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Furthermore, Shulman added, recent studies have demonstrated an important role of hepatic steatosis in causing insulin resistance in the liver, resulting in increased liver production of glucose, and high blood sugar in patients with type 2 diabetes.
"Through noninvasive measurements of hepatic triglyceride content in humans, we've learned that elevated liver fat is fairly ubiquitous in patients with poorly controlled type 2 diabetes," Shulman said. "It's been an underappreciated aspect of the disease."
Continue Reading Below ↓↓↓
The researchers examined whether or not mice deficient for the mtGPAT1 enzyme would be protected from fatty liver and liver insulin resistance. Previous studies suggested that mtGPAT1 might act as a valve, channeling certain fatty acids into the manufacture of lipid metabolites with suggested links to insulin resistance, Shulman explained.
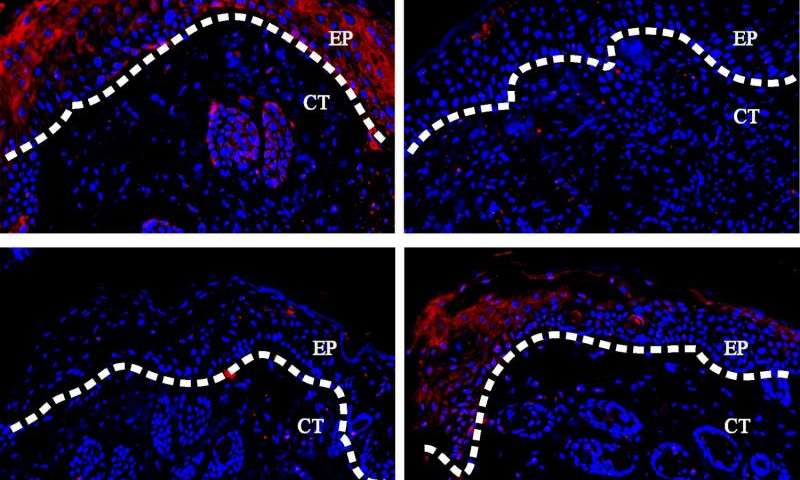
After three weeks on a high-fat diet, mice lacking mtGPAT1 had markedly lower than normal concentrations of the liver lipid metabolites hepatic triacylglycerol and diacylglycerol, the researchers reported. Compared to normal mice, the animals also were protected from hepatic insulin resistance.
Surprisingly, Shulman said, mice lacking mtGPAT1 exhibited increased hepatic insulin sensitivity despite an almost 2-fold elevation in hepatic acyl-CoA concentrations, a compound which had also been implicated in insulin resistance previously. The finding suggests that long chain acyl-CoAs do not mediate fat-induced hepatic insulin resistance.
"Protection of fat-induced hepatic insulin resistance was correlated with reduced concentrations of diacylglycerol in the liver and reduced activation of protein kinase C[epsilon]. Diacylglycerol is an important activator of protein kinase C[epsilon] and previous studies by the Shulman group have implicated activation of this kinase in hepatic insulin resistance," he explained.
"Taken together, these data implicate diacylglycerol in the liver as an important trigger in causing fat-induced hepatic insulin resistance," Shulman said. "These data also suggest that mtGPAT1 might be a potent therapeutic target to treat hepatic steatosis and hepatic insulin resistance," he added.
The researchers include Susanne Neschen, Katsutaro Morino, and Gerald I. Shulman of Howard Hughes Medical Institute, Yale University School of Medicine, New Haven, Connecticut; Linda E. Hammond and Rosalind A. Coleman of University of North Carolina, Chapel Hill, North Carolina; and Dongyan Zhang, Zhen-Xiang Liu, Anthony J. Romanelli, Gary W. Cline, Rebecca L. Pongratz, Xian-Man Zhang, and Cheol S. Choi of Yale University School of Medicine, New Haven, Connecticut. This work was supported by grants from the National Institutes of Health. G.I.S. is the recipient of a Distinguished Clinical Scientist Award from the American Diabetes Association and an Investigator of the Howard Hughes Medical Institute.
Neschen et al.: "Prevention of hepatic steatosis and hepatic insulin resistance in mitochondrial acyl-CoA:glycerol-sn-3-phosphate acyltransferase 1 knockout mice." Publishing in Cell Metabolism, Vol. 2, July 2005, pages 55-65. DOI 10.1016/j.cmet.2005.06.006. www.cellmetabolism.org
Source: Cell Press