Twin epidemics of obesity and type 2 diabetes are bearing down on the world's population, threatening the lives of hundreds of millions of people. But scientists are still trying to determine how the two conditions are linked, and what it takes to turn an obese person into a person with diabetes.
Researchers at the University of Michigan and Harvard University report new evidence in mice that may help explain that link -- and may help them understand why some obese people never develop diabetes while many others do.
The study, published in Cell Metabolism, suggests that the hormone leptin regulates blood sugar through two different brain-body pathways: One that controls appetite and fat storage, and another that tells the liver what to do with its glucose reserves.
It's already known that disrupting leptin's appetite-controlling role leads to obesity, and that obesity is known to significantly raise the risk of diabetes. But the new result suggests it may take disruptions to both pathways to bring on full-blown diabetes and overwhelm the body's ability to control blood glucose levels via the action of insulin.
The researchers, led by senior author Martin G. Myers, Jr., M.D., Ph.D., of the U-M Medical School, have spent several years exploring the exact cell-signaling mechanisms by which leptin exerts its influence on the body.
Continue Reading Below ↓↓↓
The new research is based on mice that the researchers genetically modified to disable the leptin-STAT3 cell-signaling pathway that leads from the brain to the body. The mice, called the s/s strain, could still produce both leptin and the receptor it binds to when sending STAT3 signals to the body.
The s/s mice ate too much and became obese, but they did not develop diabetes even after six months, a long time for a mouse. Meanwhile, other strains of mice that made no leptin, or have no leptin receptors, all became obese and died of diabetes.
"The blood sugar of the s/s mice was high, but it was much more in control than mice that had no leptin receptors at all, and was not because of differences in their insulin production," says Myers. "And when the s/s mice were put on calorie-restricted diets, their blood sugar normalized. These findings suggest that since the leptin-STAT3 signal was disrupted, some other signal must have been keeping glucose in check."
That other signaling pathway, though still unknown, likely controls the release of stored glucose from the liver, since that's the only other major source in the body.
That brain-liver leptin signal pathway, for which the U-M/Harvard team is already searching, is involved in glucose homeostasis, or the regulation of blood sugar by feedback loops, says Myers.
If there's a lot of sugar in the blood, homeostatic processes would keep the liver from releasing glucose by tapping into its stored-up supply of glucagon, or long-chain sugar. But if blood sugar gets low, the liver might get a signal to release some of its sugar.
Myers has been pursuing the leptin-diabetes signaling link for several years, together with the new paper's lead author and former U-M assistant research scientist Sarah H. Bates, Ph.D., who is now at University College London. The work began when Myers and Bates were at the Joslin Diabetes Center at Harvard University; their two co-authors on the new paper, Rohit Kulkarni and Matthew Seifert, are at Joslin.
The balance of sugar release from the liver, and sugar intake from the diet, is crucial to type 2 diabetes and its precursor conditions, impaired glucose tolerance and insulin resistance.
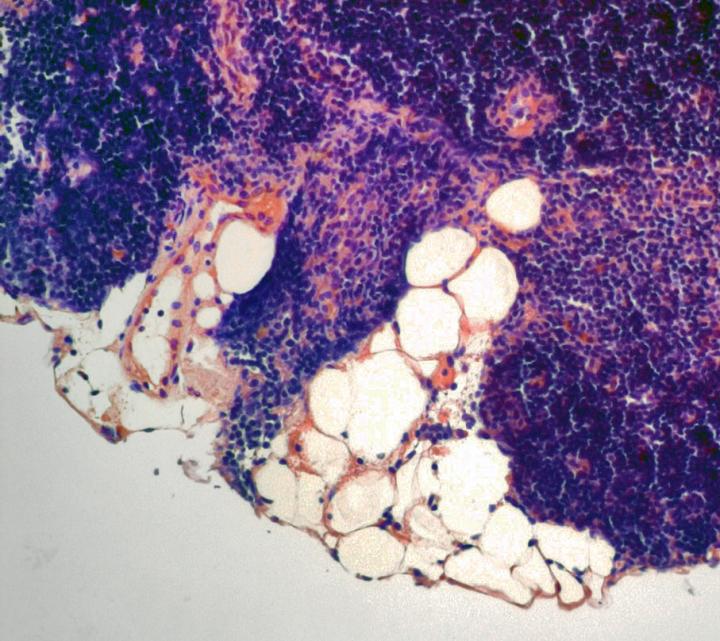
A person who has so-called "pre-diabetes" has overly high levels of blood sugar, as the beta islet cells in his or her pancreas struggle to make enough insulin. (Insulin ushers sugar into cells so it can be burned as fuel.) People with full-blown diabetes have lost that fight between insulin and sugar, and their insulin supply falls woefully short as their stressed beta islet cells begin to die.
In the new study, there was no difference in the function of islet beta cells between the s/s mice and the mice with no leptin receptors. That doesn't mean that defects in those cells aren't also involved in causing or exacerbating the slide into diabetes, Myers says.
Continue Reading Below ↓↓↓
The new paper is the latest in a string published since the s/s mouse model was developed. In early 2003, Myers' team published findings in the journal Nature that showed the s/s mice would overeat and become obese, and have other problems with their neuroendocrine system, but would not lose their ability to reproduce. This was the first time that STAT3 signaling was implicated in obesity.
The mice are so-called "knock-in" mice, because the scientists had introduced a gene mutation that interfered with the ability of the leptin receptor to initiate STAT3 signals after leptin had bound to the receptor. The other mice used in the team's studies are "knock-out" mice, in which the gene that encodes leptin, or the gene that encodes the leptin receptor, is deactivated.
In December, 2004, the team published findings about the s/s mice that showed they were more active and had more lean body mass than the mice that lacked the leptin receptor. This result showed that leptin-STAT3 signaling is critical for regulating the body's use of energy, because both types of mice were otherwise similar in their dysfunctional neuroendocrine systems.
"Taken together, our findings show there's more to the obesity-diabetes link than the classic thinking that if you eat too much sugar, you'll get fat and get diabetes -- and that if you don't get diabetes, it's only because you're making more insulin to keep up with the sugar," says Myers. "There's something else contributing. Now the challenge is to find out what that is."
He notes that the study will continue in mice, because of the difficulty in studying brain-body cell signaling in humans -- which would require a brain biopsy. But building a better understanding of the basic mechanisms involved in the diabetes-obesity link will ultimately help humankind's struggle to contain two looming health epidemics.
The research is funded by the National Institutes of Health (NIH R01 DK57631, R01 DK57768) and the American Diabetes Association. Reference: Cell Metabolism, Vol 1, No. 3, pp. 169-178, March 2005
Source: University of Michigan Health System