A recent study shows that interventional radiologists can use an innovative technique to relieve the pain that plagues millions of amputees, many of which are people with diabetes.
A pioneering technique significantly reduces phantom limb pain — chronic pain emanating from the site of amputated limbs — according to findings presented at the Society of Interventional Radiology’s 2016 Annual Scientific Meeting.
The study indicates that interventional radiologists applying cryoablation therapy, a minimally invasive targeted treatment using cold blasts, show promise in improving the quality of life for patients suffering phantom limb pain.
About 60% of non-traumatic lower-limb amputations among people over the age of 20 occur in those diagnosed with diabetes. In 2010, that amounted to about 73,000 people.
“Until now, individuals with phantom limb pain have had few medical interventions available to them that resulted in significant reduction in their pain,” said J. David Prologo, M.D., assistant professor in the division of interventional radiology at Emory University School of Medicine. “Now, with the promise of cryoablation, these individuals have a viable treatment option to target this lingering side effect of amputation–a condition that was previously largely untreatable.”
Military veterans wounded in combat and people with complex medical conditions, such as uncontrolled diabetes, constitute a significant part of the population affected by pain that seems to originate from the lost limb.
Continue Reading Below ↓↓↓
Millions of people in the U.S. live with amputated limbs and, according to the Centers for Disease Control and Prevention, nearly 200,000 amputations occur each year.
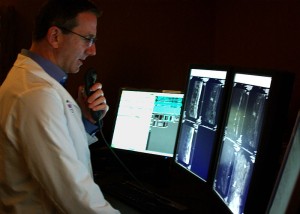
The interventional radiology team at Emory University treated 20 patients, with each person undergoing image-guided cryoablation of the nerve and scar tissue in the residual limb (the part of the body that remains after an amputation has been performed).
During cryoablation, a probe is precisely placed through the skin and the temperature is dropped for 25 minutes to create an ablation zone, shutting down nerve signals.
Researchers asked patients to rate their pain on a visual analog scale (VAS) that ranged from 1 (not painful) to 10 (extremely painful) before, seven days after and 45 days after the intervention. Before cryoablation, patients reported an average pain score of 6.4 points. By day 45, the average score was 2.4 points.
“Many of the nerves contributing to these pains are inaccessible to physicians without image guidance,” added Prologo. “With the interventional radiologist skill set, we can solve tough problems through advanced image-guided therapies, and this promising treatment can target hard-to-find nerves and help amputees dramatically improve their lives–all in an outpatient setting.”
Investigators at Emory will continue to examine the potential of this emerging intervention by tracking its effectiveness at six months after treatment and beyond. Prologo says the group has applied for a Department of Defense grant in the hopes of benefitting the thousands of veterans who have had limbs amputated and may suffer with phantom limb pain.
Abstract 408: “Percutaneous Image-Guided Cryoablation for the Treatment of Phantom Limb.” J. D. Prologo, C. Gilliland, F. Edalat, R. W. Bittman, P. Harkey, L. Brewster, Emory University School of Medicine; K. Yamada, Harvard Medical School; D. Corn, Case Western Reserve School of Medicine. SIR Annual Scientific Meeting, April 2-7. This abstract can be found at sirmeeting.org.
Source: Society of Interventional Radiology
Photo Credit: Zackstarr/WikiMedia