April 2006 - Researchers have now carefully crafted a combination therapy that reverses recent-onset type 1 diabetes in 2 animal models of disease. By combining an oral with an intranasal therapy for type 1 diabetes that have individually shown beneficial, but limited, effects in previous studies, Matthias von Herrath and colleagues at the La Jolla Institute for Allergy and Immunology deliver a one-two punch, and prove that, in this case, 2 treatments work together better than one. The study appears online on April 20 in advance of print publication in the May issue of the Journal of Clinical Investigation.
In patients with type 1 diabetes, the autoimmune response destroys insulin-producing cells (beta cells) in pancreatic islets, thereby subjecting these individuals � often children or young adults � to a lifetime of insulin injections. To prevent disease, autoreactive immune cells need to be suppressed or eliminated without negative side-effects. One treatment strategy that has been shown to suppress beta cell killing is the delivery of an antibody against the CD3 molecule expressed on most T cells. This antibody promotes the function of regulatory T cells (Tregs), which put the brakes on an overaggressive immune response. However, chronic "body-wide" suppression of the immune system in this way puts patients at risk for malignancies or reactivation of dormant viral infections, consequently dampening enthusiasm for this monotherapeutic approach.
One of the critical questions that has remained is how do we prevent immune responses against only insulin-producing cells? Promising data in animal models has shown that it is possible to deliver beneficial immune modulatory molecules to the pancreatic islets by inducing islet antigen�specific Tregs. However, this intervention only appears effective early in the pre-diabetic stage.
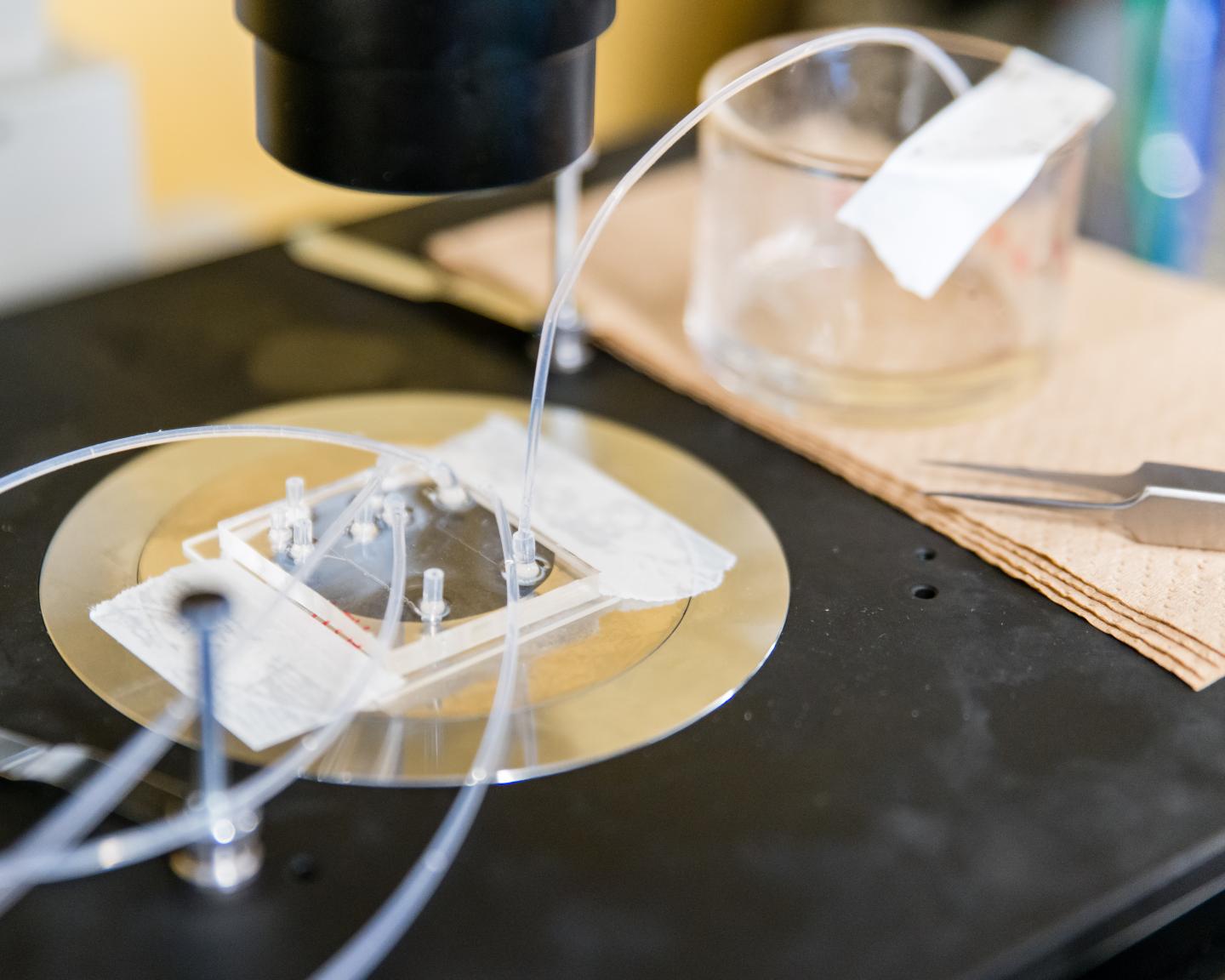
In their JCI study, von Herrath and colleagues show that combination treatment with a low-dose, orally-delivered CD3epsilon-specific antibody as well as an intranasally-delivered proinsulin peptide synergizes to reverse recent-onset type 1 diabetes in mice, with much greater efficacy than monotherapy with anti-CD3 or peptide alone.
As the induced Tregs acted to specifically shield islets from autoimmune destruction, and only a low dose of anti-CD3 antibody was required, this strategy is also expected to reduce the potential for adverse side effects resulting from the immune suppression. Suppression of the immune response in this way promotes pancreatic beta cell regeneration through the natural regenerative process.
Continue Reading Below ↓↓↓
If similar success is observed in humans, this dynamic therapeutic duo may hold great potential for the treatment of individuals with recent-onset type 1 diabetes.
TITLE: Anti-CD3 and nasal proinsulin combination therapy enhances remission from recent-onset autoimmune diabetes by inducing Tregs.
Source: Journal of Clinical Investigation