Rare benign tumors known as insulinomas contain a complicated wiring diagram for regeneration of insulin-producing human beta cells, which may hold the key to diabetes drug development, researchers at the Icahn School of Medicine at Mount Sinai report.
The study, titled “Insights into Beta Cell Regeneration for Diabetes via Integration of Molecular Landscapes in Human Insulinomas,” was published in a study in Nature Communications.
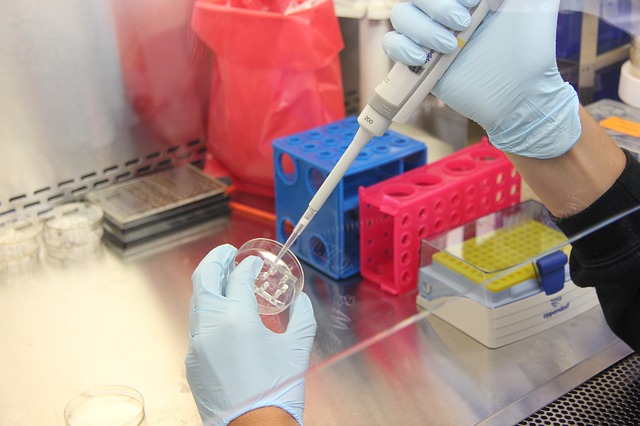
With the help of an international group of investigators, the Mount Sinai team collected 38 human insulinomas — rare pancreatic tumors that secrete too much insulin — and analyzed their genomics and expression patterns.
“For the first time, we have a genomic recipe — an actual wiring diagram in molecular terms that demonstrates how beta cells replicate,” said Andrew Stewart, MD, Director of the Diabetes, Obesity, and Metabolism Institute at the Icahn School of Medicine and lead author of the study.
Approximately 30 million people living in the United States have diabetes and nearly 50 to 80 million are living with prediabetes.
Diabetes occurs when there are not enough beta cells in the pancreas, or when those beta cells secrete too little insulin, the hormone required to keep blood sugar levels in the normal range.
Continue Reading Below ↓↓↓
Diabetes can lead to major medical complications: heart attack, stroke, kidney failure, blindness, and limb amputation.
Loss of insulin-producing beta cells has long been recognized as a cause of type 1 diabetes, in which the immune system mistakenly attacks and destroys beta cells.
In recent years, researchers have concluded that a deficiency of functioning beta cells also contributes importantly to type 2 diabetes — the primary type that occurs in adults. Thus, developing drugs that can increase the number of healthy beta cells is a major priority in diabetes research.
“When you think of tumor genomics, you’re thinking of breast cancer or colon cancer, leukemia, et cetera. No one is thinking of doing genomics on tumors that don’t really kill people,” said Dr. Stewart. “So the real innovation here is that we collected benign tumors that don’t metastasize and don’t cause great harm, and we’re trying to use these benign tumors that have beta cell regeneration going on in them, as the only reasonable source of genomic information on how to make beta cells regenerate.”
Knowing where to look is one thing, but in the era of big data, knowing how to look is very important, said Carmen Argmann, PhD, Associate Professor of Genetics and Genomic Sciences at the Icahn School of Medicine at Mount Sinai and co-author of the paper.
“In this case, we looked at millions of data points collected in rare human insulinomas to try and find an answer to a common disease, diabetes. We then computationally created two molecular pictures from that data, one from the insulinoma and one for the normal beta cell, and identified the critical differences that will hopefully lead to new ways to expand beta cell mass in diabetes patients. We plan to explore clinical applications of these new findings in close collaboration with the team at Sema4, a company specializing in big data analytics for diagnostic development.”
In 2015, Dr. Stewart and his team published a paper in Nature Medicine showing that the drug harmine drove the sustained division and multiplication of adult human beta cells in culture, a feat that had eluded the field for years. In addition, they also learned that harmine treatment tripled the number of beta cells and led to better control of blood sugar in three groups of mice engineered to mimic human diabetes.
According to Dr. Stewart, the results of the harmine study provided a large body of evidence demonstrating that the harmine drug class can make human beta cells proliferate at levels that may be relevant for diabetes treatment. The new results confirm that harmine is one pathway to beta cell regeneration but also suggest a number of new pathways that can be treated with novel diabetes drugs.
“We are excited and gratified by these remarkable results, which reveal an extraordinary array of new and validated pathways for diabetes drug development,” said Dennis S. Charney, MD, Anne and Joel Ehrenkranz Dean, Icahn School of Medicine at Mount Sinai. “In a very short time, we have made terrific progress, and it is really a credit to the remarkably diverse areas of strength in biomedical research at Mount Sinai. It is truly an exciting set of discoveries for the field of diabetes.”
This work was supported by NIDDK grants UC4 DK104211 and P-30 DK 0205241. It was also supported by the New Jersey based Foundation for Diabetes Research and by the National Institute of Health.
Continue Reading Below ↓↓↓
Also making key research contributions were Huan Wang, PhD; Aaron S. Bender BA; Peng Wang, PhD; Esra Karakose, PhD; William B. Inabnet, MD; Donald K. Scott, PhD; Gustavo Fernandez-Ranvier, MD; Bojan Losic, PhD; Rong Chen, PhD; Yevgeniy Antipin MS; Luca Lambertini, PhD, Milind Mahajan, PhD; Yayoi Kinoshita, DDS; Michael J. Donovan, PhD, MD; Andrew Uzilov, PhD; Boris Reva, PhD; and Eric E. Schadt, PhD, from the Icahn Institute of Genomics and Multiscale Biology; the Diabetes, Obesity, and Metabolism Institute; the Department of Surgery; and the Department of Pathology at the Icahn School of Medicine at Mount Sinai, and Sema4. Additional investigators from around the United States, Europe, and China were instrumental in supporting the study.
The Mount Sinai Hospital / Mount Sinai School of Medicine: Rare benign tumors hold the ‘genetic recipe’ to combat diabetes
Journal: Nature Communications