A new, minimally invasive transplant technique has restored natural insulin production in a woman with Type 1 Diabetes. She is now completely off insulin and has an excellent glucose profile.
The Diabetes Research Institute (DRI), a Center of Excellence at the University of Miami Miller School of Medicine, announced today that the first patient in its clinical trial has been free from insulin injections in record time following the implantation of islet cells within a biological scaffold.
The patient, Wendy Peacock, 43, from San Antonio, TX, underwent the minimally invasive procedure on August 18, 2015, and is now producing her own insulin naturally for the first time since being diagnosed with type 1 diabetes at age 17.
In this pilot study, DRI researchers are testing a new transplant technique for insulin-producing cells, building upon decades of progress in clinical islet transplantation.
This trial is an important first step toward the development of the DRI BioHub, a bioengineered mini-organ that mimics the native pancreas to restore natural insulin production in people with type 1 diabetes.
 “The first subject in our Phase I/II pilot BioHub trial is now completely off insulin with an excellent glucose profile. These are the best post-transplant results we’ve seen in an islet recipient,” said Camillo Ricordi, MD, director of the DRI and the Stacy Joy Goodman Professor of Surgery, Distinguished Professor of Medicine, Professor of Biomedical Engineering, Microbiology and Immunology at the University of Miami Miller School.
“The first subject in our Phase I/II pilot BioHub trial is now completely off insulin with an excellent glucose profile. These are the best post-transplant results we’ve seen in an islet recipient,” said Camillo Ricordi, MD, director of the DRI and the Stacy Joy Goodman Professor of Surgery, Distinguished Professor of Medicine, Professor of Biomedical Engineering, Microbiology and Immunology at the University of Miami Miller School.
Continue Reading Below ↓↓↓
Dr. Ricordi also serves as director of the DRI’s Cell Transplant Center. “This was the first tissue engineered islet transplant using a ‘biodegradable scaffold’ implanted on the surface of the omentum.
The technique has been designed to minimize the inflammatory reaction that is normally observed when islets are implanted in the liver or in other sites with immediate contact to the blood.
If these results can be confirmed, this can be the beginning of a new era in islet transplantation. Our ultimate goal is to include additional technologies to prevent the need for life-long anti-rejection therapy,” Dr. Ricordi added.
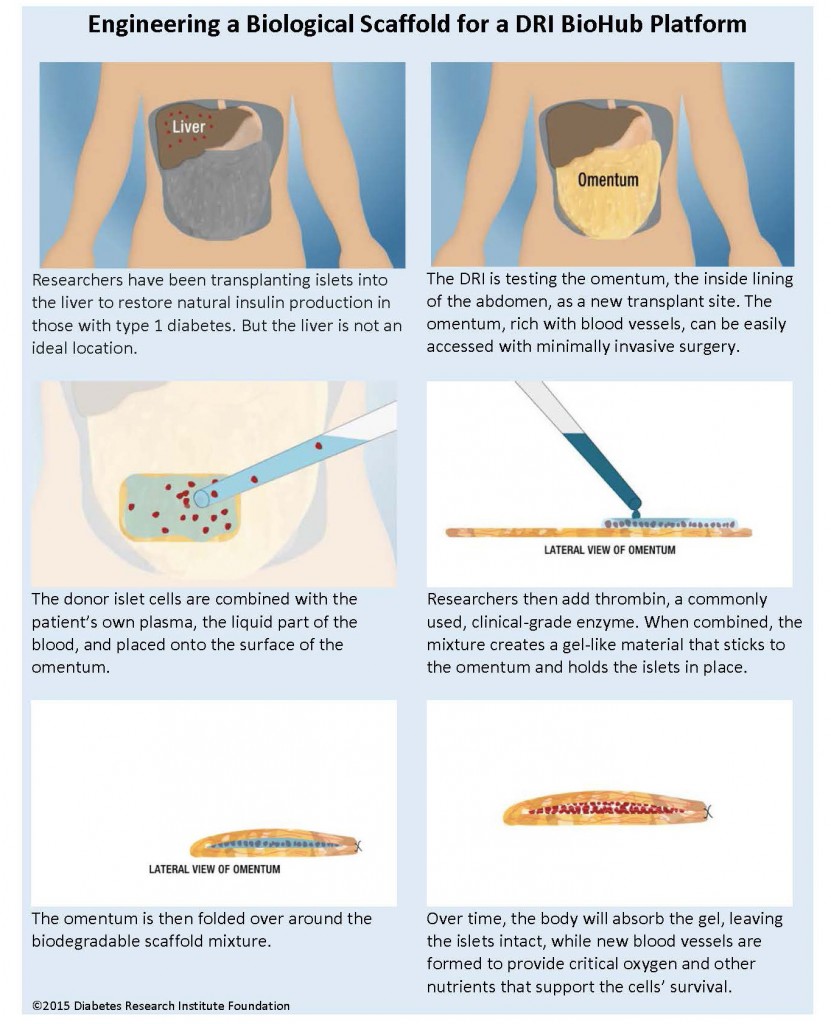
The omentum is a highly vascularized tissue covering abdominal organs. The donor islets were implanted within a biodegradable scaffold, one of the platforms for a DRI BioHub, made by combining the patient’s own blood plasma with thrombin, a commonly used, clinical-grade enzyme.
Together, these substances create a gel-like material that sticks to the omentum and holds the islets in place. The omentum is then folded over around the biodegradable scaffold mixture. Over time, the body will absorb the gel, leaving the islets intact, while new blood vessels are formed to provide critical oxygen and other nutrients that support the cells’ survival.
This pilot trial will include the immunosuppressive regimen currently used for clinical islet transplantation studies and will be limited to a small group of participants (See Graphic Below).

 “As any type 1 knows, you live on a very structured schedule. I do a mental checklist every day in my head…glucose tabs, food, glucometer, etc., and then I stop and say, ‘WOW! I don’t have to plan that anymore.’ Laying down at night and going to sleep and not having to worry about lows is something that is so foreign to me. It’s surreal to me…I’m still processing the fact that I’m not taking insulin anymore,” said Peacock, who was a candidate for the DRI’s clinical trial because she suffered with severe hypoglycemia unawareness, a complication of diabetes in which patients are unable to sense that their blood glucose is dropping to dangerously low levels. People with hypoglycemia unawareness often become disoriented, lose consciousness or go into convulsions. It may even lead to death.
“As any type 1 knows, you live on a very structured schedule. I do a mental checklist every day in my head…glucose tabs, food, glucometer, etc., and then I stop and say, ‘WOW! I don’t have to plan that anymore.’ Laying down at night and going to sleep and not having to worry about lows is something that is so foreign to me. It’s surreal to me…I’m still processing the fact that I’m not taking insulin anymore,” said Peacock, who was a candidate for the DRI’s clinical trial because she suffered with severe hypoglycemia unawareness, a complication of diabetes in which patients are unable to sense that their blood glucose is dropping to dangerously low levels. People with hypoglycemia unawareness often become disoriented, lose consciousness or go into convulsions. It may even lead to death.
“We’re quite excited. This has been the best outcome we have seen at this stage. It’s a unique site, the surgery is very simple and the patient recovers very quickly. We will continue until our final goal – islet transplantation without immunosuppression,” adds Rodolfo Alejandro, MD, Professor of Medicine and director of the DRI Clinical Cell Transplant Program.
In type 1 diabetes, the insulin-producing islets cells of the pancreas have been mistakenly destroyed by the immune system, requiring patients to manage their blood sugar levels through a daily regimen of insulin therapy.
Continue Reading Below ↓↓↓
Islet transplantation has allowed some patients to live without the need for insulin injections after receiving a transplant of donor cells. Some patients who have received islet transplants at the DRI have been insulin independent for more than a decade, as DRI researchers have published.
Currently, islet cells are infused into the liver, but many of the cells do not survive in that environment. “The liver is a very simple site to access, but we have known for years that it’s not the ideal site. And the liver will not accommodate a device for housing the islets,” explained Dr. Alejandro.
To learn more about the DRI’s clinical trial and the transplant procedure, please click here.
The research projects that comprise the DRI BioHub receive philanthropic support from the Diabetes Research Institute Foundation. Funding for the DRI BioHub is also provided by other sources, including JDRF, The Leona M. and Harry B. Helmsley Charitable Trust, National Institutes of Health (NIH), NIH Small Business Innovation Research (SBIR), University of Miami, pharmaceutical companies, and additional corporate and philanthropic partners. For more information on the development, visit BioHub.
About the Diabetes Research Institute
The Diabetes Research Institute at the University of Miami Miller School of Medicine leads the world in cure-focused research. As the largest and most comprehensive research center dedicated to curing diabetes, the DRI is aggressively working to develop a biological cure by restoring natural insulin production and normalizing blood sugar levels without imposing other risks. Researchers have already shown that transplanted islet cells allow patients to live without the need for insulin therapy. The DRI is now building upon these promising outcomes by developing the DRI BioHub and is testing various BioHub platforms in preclinical and clinical studies. For more information, please visit DiabetesResearch.org or call 800-321-3437. You can tweet DRI at @Diabetes_DRI.
Acknowledgements
The Diabetes Research Institute Foundation would like to acknowledge and thank all of those who contributed to this clinical trial, including the Clinical Islet Transplant Team, the DRI cGMP Team, the Miami Transplant Institute, Jackson Health System, the University of Miami Miller School of Medicine, the Life Alliance Organ Recovery Agency and the DRI Preclinical Research Teams.